- Review
- Open access
- Published:
CRISPR/Cas-based CAR-T cells: production and application
Biomarker Research volume 12, Article number: 54 (2024)
Abstract
Chimeric antigen receptor T cell (CAR-T) therapy has revolutionized the treatment approach for cancer, autoimmune disease, and heart disease. The integration of CAR into T cells is typically facilitated by retroviral or lentiviral vectors. However, the random insertion of CARs can lead to issues like clonal expansion, oncogenic transformation, variegated transgene expression, and transcriptional silencing. The advent of precise gene editing technology, like Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), allows for controlled and precise genome modification, facilitating the translation of CAR-T research to the clinical applications. This review aims to provide a comprehensive analysis of the application of CRISPR gene editing techniques in the context of precise deletion and insertion methodologies, with a specific focus on their potential for enhancing the development and utilization of CAR-T cell therapy.
Introduction
Overview of CAR-T cell therapy
Chimeric antigen receptor T cell (CAR-T) cell therapy has demonstrated remarkable efficacy and safety for the treatment of hematological malignancies in recent years. CAR constructs, which consist of an extracellular antigen-binding domain (single-chain fragment variable, scFv), transmembrane hinges, and intracellular signal domains (such as CD3ζ chain and costimulatory domain), enable CAR-T cells to specifically identify, activate, and eradicate tumor cells in an antigen-specific and MHC-independent manner [1]. So far, six CAR-T products leveraging this mechanism have been approved for the therapeutic management of B-cell acute lymphoblastic leukemia/Non-Hodgkin Lymphoma (B-ALL/NHL) or Multiple Myeloma (MM). However, the production of all six products involves the introduction of CAR genes into human primary T cells through infection with lentivirus (LV) or retroviral vector (RV). Consequently, this integration process may result in clone amplification, carcinogenic transformation, mutated transgenic expression, and transcriptional silencing. Additionally, CAR-T cell exhaustion, toxicity concerns, and limited autologous cell availability have hindered widespread adoption.
Briefs of gene editing technologies
Gene editing technologies play a crucial role in the production and optimization of CAR-T cells for anti-tumor purposes. These technologies, including transcription activator-like effector nucleases (TALENs), zinc-finger nucleases (ZFNs), and clustered regularly interspaced short palindromic repeats (CRISPR), facilitate precise modification and manipulation of genes in CAR-T cell engineering [2].
ZFNs and TALENs are chimeric nucleases comprising a modular DNA-binding domain and a sequence-independent cleavage domain derived from the FokΙ restriction enzyme [3]. Utilizing a zinc finger protein or transcriptional activator-like effect (TALE) domain, they recognize and bind to DNA at a specific sequence. Subsequently, they introduce an endonuclease to cleave the sequence, resulting in a DNA double-stranded break (DSB) at the targeted locus. However, the broad application of TALENs and ZFNs is hindered by the time-consuming and complex process involved, as a specific editing protein is required for each version of genome editing [4, 5]. Following the DSB, the eukaryotic cellular DNA repair system repairs the DSBs through either the homology-directed repair (HDR) or non-homologous end joining (NHEJ) pathways [6], leading to targeted integration or disruption of genes, depending on the pathway utilized.
In contrast, the CRISPR/Cas system is widely recognized as a powerful gene editing tool due to its simple design and high efficiency, offering promising prospects for cancer treatment. CRISPR/Cas system has greatly simplified the gene editing process and is now extensively applied in cell therapy, with recent progress toward clinical applications. Initially reported in E. coli, CRISPRs were later identified as an intrinsic adaptive immune system in eukaryotic cells, providing defense against foreign DNA. Currently, the most used systems are CRISPR/Cas9 and CRISPR/Cas12a. The CRISPR/Cas9 technology involves a 20-base pair single guide RNA (sgRNA) that guides the DNA endonuclease to the desired cutting site. This site is specified by a protospacer adjacent motif (PAM) sequence located downstream of the cleavage site within the target DNA [7]. On the other hand, the CRISPR/Cas12a system recognizes the TTTV sequence on the genome and requires only a single crRNA to cut the genomic DNA. This process produces sticky ends that are repaired similarly to CRISPR/Cas9. MEGA-CRISPR harnesses Cas13d’s RNA-directed editing capabilities through tailored guide RNA (gRNA) design, enabling precise recognition and cleavage of target RNA sequences for editing [8]. Here is a comparison of the advantages and drawbacks of CRISPR/Cas9, CRISPR/Cas12a, and CRISPR/Cas13d in CAR-T therapy, presented in Table 1. These characteristics help better understand the strengths and limitations of each system in the context of CAR-T therapy. The CRISPR/dCas9 system is utilized to modulate transcriptional activities by recruiting transcriptional activators or repressors to specific loci, known as CRISPR activation (CRISPRa) and CRISPR interference (CRISPRi), respectively. Provided below is an in-depth exploration regarding the generation of CAR-T cell therapy leveraging the aforementioned gene editing approaches [9].
The production of CRISPR/Cas-based CAR-T cells
Currently, there are three primary approaches for generating CAR-T cells utilizing the CRISPR system, with the most conventional being the CRISPR/Cas9 system, alongside CRISPR/Cas12a and CRISPR/Cas13d. The procedures for generating CAR-T cells utilizing these systems will be elaborated upon in the following sections.
Current state of research on the production of CAR-T cells using the CRISPR/Cas9 system
Over the years, extensive research has been undertaken to deliver the CRISPR system into human primary T cells in three different forms: (i) Viral delivery of CRISPR vectors, such as LV or adeno-associated virus (AAV), (ii) Cas9 mRNA combined with synthetic guide RNA, (iii) Binding of Cas9 protein and synthetic guide RNA to form RNP complex [10, 11] (Fig. 1). The efficiency of gene knockout using CRISPR/Cas9 gene editing is relatively high, with the efficiency at the PD-1 locus exceeding 75%. Previous researchers have integrated guide RNA and CAR into a single vector, subsequently electro-transferring Cas9 mRNA to create gene-edited CAR-T cells. The efficacy of CRISPR/Cas9-mediated knockout hinges on the choice of target and guide RNA. To enhance knockout efficiency, researchers introduced MS (2’-Omethyl 3’-phosphorothioate) or MSP (2’-O-methyl 3’-thio PACE) modifications to the guide RNA. After binding the modified guide RNA to the Cas9 protein, they electrotransfected it into human primary T cells and CD34 + hematopoietic stem cells simultaneously. The results demonstrated a 2.4-fold increase in indel frequencies for MS-modified sgRNAs compared to unmodified ones (30.7% vs. 12.8%), significantly improving genome editing efficiency [12].
CRISPR mediate gene KO and KI strategy in CAR/TCR-T cell therapy. To achieve the formation of CAR/TCR-T cells, sgRNA and Cas9 protein are co-transposed into T cells, while CAR/TCR can enter T cells through two primary methods, eventually resulting in CAR/TCR-T cells. (1) Random insertion via LV/RV: The CAR or TCR is randomly inserted into T cells using LV or RV. (2) Precise insertion: This method facilitated by a donor template. Various forms of templates such as dsDNA, ssDNA, pDNA, or AAV are employed for site-specific integration of CAR or TCR into the T cells. sgRNA, single guide RNA; LV, lentivirus; RV, retrovirus; KO, knockout; KI, knockin; dsDNA, double strain DNA; ssDNA, single strain DNA; pDNA, plasmid DNA; AAV, Adeno-associated virus
Current research on CAR-T cell production using the CRISPR/Cas12a system
Cas12a (Cpf1) has two major isoforms, AsCpf1 and LbCpf1, known for higher specificity toward human cells compared to Cas9. It is now understood that Cas12a cleaves genomic DNA, generating sticky ends and displaying greater susceptibility to homologous recombination repair [13]. AAV6 vectors have been employed to engineer CrTRAC, crPDCD1, and CD19 CAR into one vector, achieving a simultaneous knockin efficiency of 37%, seven times that of the CRISPR/Cas9 system. The AAV-Cpf1 KIKO system established a precedent for the efficient expression of two CARs in the same T cell, facilitating the clinical application of bispecific CAR-T cells. Despite high gene knockin and knockout efficiency, Cas12a RNP cleavage efficiency was relatively low [14]. Researchers addressed this by developing a mutated version, AsCas12a Ultra, carrying M537R and F870L mutations. These mutations significantly enhanced knockout and knockin efficiency, especially in T cells, with single transgene knockin reaching up to 60% and double knockin up to 40% [15].
Current research on CAR-T cell production using the CRISPR/Cas13d system
Tieu et al. introduced MEGA-CRISPR, a CRISPR/Cas13d-based tool [8], which utilizes tailored gRNA design to edit target RNA sequences with precision. This technology shows promise in enhancing CAR-T cell therapy efficacy by addressing T cell exhaustion and improving anti-cancer capabilities within the tumor microenvironment. Empirical validation in murine models demonstrates MEGA-CRISPR’s ability to enhance tumor cell killing efficiency, leading to significant tumor suppression and prolonged survival. Despite its potential, challenges such as complex technology and safety assessment hinder its widespread use. Further research and clinical validation are necessary to optimize MEGA-CRISPR for clinical applications.
CRISPR/Cas system-mediated loci-specific knockin in CAR-T cells
To date, CAR-T cells have been primarily transduced using γ-retroviral vectors or lentiviral vectors. However, these methods result in random DNA integration in T cells and carry the risk of malignant transformation. To overcome this problem, one intriguing strategy is site-specific gene integration. By utilizing target-directed nucleases to create a double-strand break at a specific genomic locus, CAR transgenes can be integrated into the T cell genome via homologous recombination.
In 2017, Michel Sadelain’s group employed knockin techniques to insert the CD19 CAR gene into the TRAC locus, generating TRAC CAR-T cells. In comparison to CAR-T cells infected with retroviral vectors, the CD19 CAR knockin CAR-T cells exhibited diminished differentiation and depletion, while demonstrating significantly improved anti-tumor effects in mouse models [16]. In a melanoma mouse model, TCR-T cells generated with linear double-stranded DNA (dsDNA) as an HDR template exhibited more pronounced inhibition of melanoma growth compared to TCR-T cells generated with lentiviral vectors [10]. By utilizing non-viral, gene-specific targeted CAR-T cells through CRISPR-Cas9 at the PD-1 locus, it was demonstrated that non-viral, gene-specific integrated CAR-T cells offer both high safety and efficacy. This provides an innovative technology for CAR-T cell therapy of B-ALL [17]. A novel approach was devised to create targeted knockin CAR-T cells by employing modified plasmid DNA as a donor (referred to as pTRAC-CAR-T cells). In a murine leukemia model, the anti-tumor efficacy of these pTRAC-CAR-T cells was assessed and compared with CAR-T cells generated using AAV as the donor template. Results indicated that both variants of CAR-T cells demonstrated comparable anti-tumor effects. The well-established and cost-effective GMP (Good Manufacturing Practice) production of plasmid vectors highlights the feasibility of leveraging pTRAC-CAR-T cells generated from plasmid templates through the CRISPR/Cas9 system for prompt integration into future clinical trials [18].
In summary, there are presently three primary HDR template types for targeted gene delivery into primary T cells using the CRISPR system: (1) AAV-dependent target gene delivery [14, 16]; (2) linear ssDNA/dsDNA target gene delivery [10, 19]; and (3) plasmid DNA target gene delivery (Fig. 1). When employing AAV6 for target genes, one method involves co-transferring synthetic guide RNA and Cas9 mRNA via electrotransfer into human primary T cells, specifically targeting the TRAC site, followed by the introduction of AAV6 carrying the CAR gene. This approach achieves an editing efficiency of up to 45.6% [16]. An alternative strategy involves designing the guide RNA, purifying the Cas9 protein, creating an RNP complex in vitro, electrotransfecting it into T cells, and subsequently introducing AAV6 carrying the CAR gene. Using this method, the knockin efficiency can reach approximately 50% in T cells. In instances where linear dsDNA is utilized for knockin into the TRAC or PD-1 locus of human primary T cells, the knockin efficiency of the CAR/TCR gene is approximately 10-20% [10, 17]. Plasmid vectors, employed as HDR templates with the CRISPR/Cas9 system, necessitate the incorporation of a guide RNA sequence at each end of the homologous arm of the target gene, in addition to vectors containing guide RNA. The presence of the vector containing guide RNA significantly enhances the knockin efficiency, resulting in a 4-8-fold increase compared to the vector without guide RNA [18]. Both the advantage and disadvantage were showed in Table 2.
The application of CRISPR/Cas-based CAR-T cells
The utilization of CRISPR-based CAR-T cells encompasses several key facets, including the generation of universal CAR-T cells, overcoming immune checkpoint inhibition, and mitigating CAR-T cell fratricide. Subsequently, a detailed exploration of the application of CRISPR-based CAR-T cells in both scientific investigation and clinical settings will be provided.
Generation of universal CAR-T cells
Currently, most CAR-T cell manufacturing relies on T cells sourced from autologous peripheral blood mononuclear cells (PBMCs). However, the costly and time-consuming production process may impede the accessibility of CAR-T cell therapy for individuals in urgent need, including those with rapidly progressing diseases or those unable to obtain potent autologous T cells due to inherent T cell defects [20]. In such scenarios, the utilization of off-the-shelf CAR-T products derived from healthy donors could potentially address these challenges. Nevertheless, the significant obstacle of acute and chronic graft-versus-host disease (GVHD) looms over this intriguing concept. To mitigate the risk of GVHD, CAR-T cells can be derived either from the patient’s previous HLA-matched hematopoietic stem cell transplant (HSCT) donor or through the genetic modification of CAR-T cells. Researchers have turned to gene editing technology to disrupt genes encoding the T cell receptor (TCR) and major histocompatibility complex (MHC), both of which contribute to alloreactivity. Two critical genes, TRAC and TRBC, encode endogenous TCR chains, with the TRAC locus serving as an ideal target for gene knockout and CAR knockin.
In addition, Georgiadis et al. pioneered the creation of TCR-knockout CAR-T cells by integrating a self-inactivating lentiviral platform with the CRISPR/Cas system. Their study demonstrated that these TT CAR-T cells exhibit superior potency compared to TCR-positive CAR-T cells. Another promising approach to diminish the allogeneic response involves the ablation of MHC class I by targeting B2M. Researchers have successfully generated TRAC, B2M, and PDCD1 multiplex knockout CAR-T cells targeting CD19 or prostate stem cell antigen (PSCA), exhibiting reduced alloreactivity coupled with enhanced anti-tumor activity [21]. (Fig. 2)
Disrupting immune checkpoint inhibitors
T cells express inhibitory receptors on their surface, contributing to T cell exhaustion, including PD-1, CTLA4, TIGIT, LAG-3, CD244, CD160, TIM3, and others. The suppressive tumor microenvironment and tumor cells can induce T cell anergy and exhaustion by upregulating inhibitory immune checkpoint signaling [22]. Repeated encounters with tumor cells lead CAR-T cells to adopt an exhausted phenotype primarily due to the upregulation of immune inhibitory receptors by tumor cells [22,23,24]. Knocking out these receptors enhances T cells’ ability to recognize tumor antigens. The PD-1/PD-L1 signaling pathway modulates T cell proliferation, activation, exhaustion, and immune tolerance [25]. Blocking the PD-1/PD-L1 axis on T cells has been documented to enhance CAR-T cell function [26, 27]. Inhibiting the expression of immunosuppressive receptors like PD-1 has been extensively studied in hematologic and solid tumors. Current evidence suggests that PD-1 knockout activates the T cell immune response against tumors, particularly in lung cancer. Additionally, PD-1 knockout has demonstrated increased anti-tumor activity in CD19 CAR-T cells for hematological malignancies, GPC3 CAR-T cells for liver cancer, and mesothelin CAR-T cells for human ductal adenocarcinoma. Knocking out molecular markers associated with T cell exhaustion, like PD-1 and CTLA4, in Universal CARs improved their tumor-killing activity. Taken together, the above findings suggest that CAR-T cell therapies designed based on immune checkpoints offer potential advantages in controlling solid tumors, presenting a novel strategy for adoptive T cell therapies.
Combining immunotherapy with CAR-T cells and immune checkpoint blockade has shown tumor regression. However, systematic administration of immune checkpoint/ligand monoclonal antibodies poses a risk of immune-related adverse events (IRAEs) [28]. Genetically disrupting intrinsic PD-1 signaling using CRISPR/Cas9 can minimize toxicity while preserving CAR-T cells’ effector function. Extensive evidence supports the idea that abrogating PD-1 with CRISPR/Cas9 enhances the anti-tumor potency of both allogeneic and autologous CAR-T cells in hematological malignancies and solid tumors during preclinical and clinical evaluations [11, 29].
To counterbalance the negative impact of the Fas/FasL axis on T cell survival, Ren et al. developed a practical one-shot CRISPR system. They incorporated multiple gRNAs into a lentiviral vector along with a CAR transgene, resulting in the generation of Fas-resistant universal CAR-T cells and PD-1/CTLA-4 dual-resistant universal CAR-T cells. Despite a decrease in knockout efficacy with an increased number of targeted genes, Fas-deficient CAR-T cells exhibited enhanced resistance to AICD, leading to prolonged persistence [30]. This finding was supported by Zhang et al., who reported robust efficacy of LAG-3-deficient CAR-T cells in a preclinical model [31]. (Fig. 2)
Avoiding fratricide in CAR-T cell therapy targeting T cell malignancy
While CAR-T cell therapy has demonstrated remarkable success in treating advanced B-cell malignancies and adult relapsed/refractory multiple myeloma, its effectiveness is currently limited, and treatment options for refractory and relapsed T cell-related tumors remain scarce. A significant challenge in CAR-T cell therapy lies in the presence of targeted T cell-pan markers on CAR-T cells, potentially resulting in self-activation, fratricide, and impaired functionality of CAR-T cells. These factors significantly impact the efficacy of CAR-T cell therapy for T cell-related tumors.
CD5 and CD7 are transmembrane proteins that are highly expressed in T cell malignancies [32, 33], with restricted expression mainly to T cells, NK cells, and B1 cells, making them attractive targets for CAR-T cell therapy. However, the presence of shared antigens on tumor cells and CAR-T cells could lead to fratricide. To mitigate this issue, researchers have explored genetic editing of the CD5 and CD7 genes in CAR-T cells using the CRISPR/Cas9 system [34].
In the development of CD5-targeted CAR-T cells for T cell malignancies, researchers encountered a challenge of self-mutilation during the in vitro generation process. To address this, they employed the CRISPR/Cas9 system to knockout CD5 on CAR-T cells. This approach resulted in reduced levels of CAR-T cell activation while significantly increasing the expression of CD5 CARs [35]. In an experiment conducted by the Carl June group, CD5 knockout CAR-T cells injected into a mouse Jurkat T tumor model led to a significant extension of the mice’s survival. Another target, CD7, exhibited high expression not only in T lymphoma cells but also in normal T cells. Knocking out CD7 using the CRISPR/Cas9 system did not impact T cell proliferation or killing ability. In an AML mouse model, tumors largely disappeared when mice were injected with CD7-knockout CAR-T cells. TCR-, β2M-, and CD7-knockout universal CAR-T cell therapy has been investigated in clinical trials for treating T cell acute lymphoblastic leukemia (T-ALL). (Fig. 2)
CRISPR/Cas9-based gene-knockout enhances CAR-T cell function
T cells express a variety of inhibitory receptors on their surface, including PD-1, CTLA4, TIGIT, LAG-3, CD244, CD160, and TIM3, contributing to T cell exhaustion [22, 23, 36]. Knocking out these receptors has been shown to enhance T cells’ ability to recognize tumor antigens. In this respect, the suppression of PD-1 expression has been extensively studied in hematological and solid tumors [25]. PD-1 knockout activates the T cell immune response against tumors, providing a potential treatment for lung cancer [37]. Moreover, PD-1 knockout enhances the anti-tumor activity of CD19 CAR-T cells in hematological malignancies. To address the negative effect of the Fas/FasL axis on T cell survival, Ren et al. developed a practical one-shot CRISPR system. Multiple gRNAs were incorporated into a lentiviral vector along with the CAR transgene, resulting in the generation of Fas-resistant universal CAR-T cells and PD-1/CTLA-4 dual-resistant universal CAR-T cells. Despite a decrease in knockout efficacy with an increasing number of targeted genes, Fas-deficient CAR-T cells demonstrated greater resistance to AICD and prolonged persistence [30]. Similarly, Zhang et al. reported robust efficacy of LAG-3-deficient CAR-T cells in preclinical models [31].
Beyond immune checkpoints, there are other molecules whose knockout can improve CAR-T cell function or reduce side effects in therapy. Fas, a member of tumor necrosis factor-alpha (TNF-α), mediates cell death through the Fas-FasL signaling-induced activation-induced cell death (AICD), potentially reducing CAR-T cell activation. Producing anti-Fas CAR-T cells using the CRISPR/Cas9 system can improve CAR-T cell tolerance to AICD and prolong the survival of tumor-bearing mice. TGF-β, binding to the TGF-β receptor (TGFBRI) on the T cell membrane, activates downstream signaling pathways SMAD2 and SMAD3, leading to reduced cytokine production and increased cytotoxicity [38]. Knocking out TGF receptor II (TGFBR2) in CAR-T cells using the CRISPR-Cas9 system promotes the differentiation of CAR-T cells into central memory and effector cells, enhancing tumor clearance in solid tumor models [39].
It has been established that adenosine, an immunosuppressive factor, activates the adenosine A2A receptor, inhibiting the activation of multiple immune cells and suppressing the anti-tumor immune response. Using CRISPR/Cas9 to knock out the adenosine A2A receptor was found to enhance the anti-tumor effects of Her2-targeted CAR-T cells in breast cancer [40]. Glycerol diglyceride kinase (DGK) metabolizes glycerol diesters into phosphatidic acid. Knocking out DGK enhances TCR signaling, increasing the killing capacity of T cells in glioma [41]. Granulocyte macrophage colony-stimulating factor (GM-CSF), mainly produced by T cells and macrophages, has been targeted in clinical trials involving leukemia patients. GM-CSF knockout, coupled with the generation of CAR-T cells targeting IL6, has been shown to reduce autocrine production of IL-1 and IL-6, subsequently decreasing cytokine release syndrome (CRS) in patients. GM-CSF knockout has also been found to enhance the anti-tumor efficacy of CD19-targeting CAR-T cells in mice, prolonging the survival time of tumor-bearing mice [42, 43]. (Fig. 2)
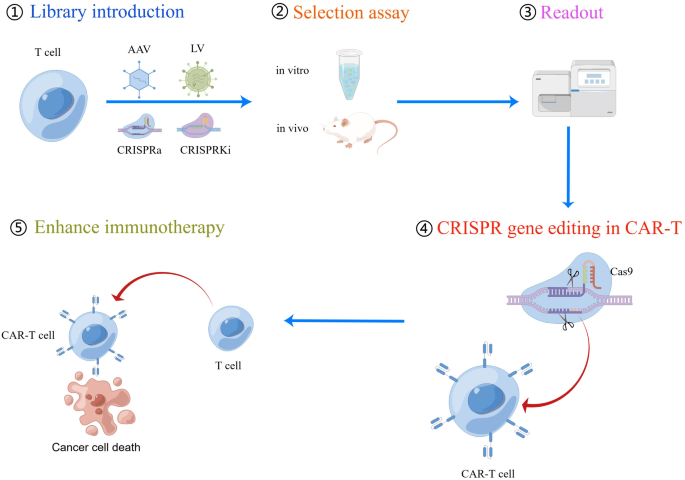
Gain of CAR-T cell function by CRISPR screening
Zhang Feng’s research group has advanced CRISPRa and CRISPRi technologies, increasingly employed for screening and modifying genes related to T cell function [44,45,46]. These technologies entail the introduction of CRISPRa and CRISPRi libraries into T cells using AAV or LV vectors. Through in vitro and in vivo experiments, target genes associated with T cell cytotoxicity are identified, enhancing the tumor-killing ability of CAR-T cells through single or multiple gene editing. This innovative technology opens new possibilities for T cell therapy (Fig. 3).
The flow chart of CRISPR screening process to screen genes to enhance CAR-T cell function. (1) CRISPRa or CRISPRi components (including guide RNA library) can be delivered into T cells using viral vectors such as AAV or lentivirus. (2) Depending on the phenotypes of interest, either in vitro or in vivo assays can be utilized for guide RNA selection. (3) Next-generation sequencing is then conducted to assess guide RNA enrichment or deletion. (4) Target gene editing is performed in T cells using CRISPR/Cas technology. (5) The ultimate objective of these screens is to evaluate the capacity to enhance the recognition and killing of tumor cells by CAR-T cells. CRISPRa, CRISPR activation; CRISPRi, CRISPR interference; AAV, Adeno-associated virus
Sidi Chen has developed a hybrid genetic screening system in which Sleeping Beauty (SB) transposons and a sgRNA cassette are nested in adeno-associated virus (AAV) [47]. This system enables efficient gene editing in primary murine T cells and provides a screening readout. In vivo, AAV–SB-CRISPR screens were conducted to identify membrane protein targets in CD8 + T cells in mouse models of glioblastoma (GBM). The screen hits, including PDIA3, MGAT5, EMP1, and LAG3 gene editing, were validated through the adoptive transfer of CD8 + T cells, enhancing the survival of GBM-bearing mice in both syngeneic and T cell receptor transgenic models [47]. In another study by Hongbo Chi et al., an in vivo pooled CRISPR-Cas9 screening system was employed to target REGNASE-1 in CD8 + T cells. The results demonstrated that CD8 + T cells with REGNASE-1 knockout exhibited long-lived effector cells with extensive accumulation, better persistence, and robust effector function in tumors [48]. Further research showed that knockout of REGNASE-1 enhances CAR-T cell persistence and CAR-T-mediated antitumor immunity in murine and human xenograft B-ALL models. This was achieved by targeting TCF7 mRNA to inhibit the formation of precursors of exhausted T cells (TPEX) [49].
Alexander Marson conducted multiple genome-wide CRISPR knock-out screens under different immunosuppressive conditions to identify genes that can be targeted to prevent T cell dysfunction. These screens revealed that RASA2, a RAS GTPase-activating protein (RasGAP), serves as a signaling checkpoint. It has been established that RASA2 is downregulated upon acute T cell receptor stimulation and gradually increases with chronic antigen exposure. Ablation of RASA2 was found to enhance MAPK signaling and CAR-T cell cytolytic activity in response to the target antigen [50]. CRISPR screening also identified that inactivating MED12 or CCNC in CAR-T cells increased T cell expansion and metabolic fitness, ultimately enhancing T cell effector activity [51].
Jeremy N. Rich et al. utilized CRISPR screening in CAR-T cells to identify the knockout of TLE4 and IKZF2, which enhanced the efficacy of CAR-T cells against glioblastoma [52]. Douglas R. Green et al. employed CRISPR screening to identify inhibitors of antigen-specific memory T cell generation in vivo. Their study revealed the crucial role of the cBAF complex in T cell fate decisions and CAR-T cells [53]. Sidi Chen’s lab devised a dead-guide RNA (dgRNA)-based CRISPR activation screen system in primary CD8 + T cells. Through this system, they identified gain-of-function targets for CAR-T engineering. They demonstrated that overexpressing PRODH2, which takes part in proline metabolism, enhances CAR-T-based killing and in vivo efficacy in various cancer models. These findings not only present a method for identifying immune boosters with gain-of-function, but also highlight PRODH2 as a target to enhance CAR-T efficacy by reshaping gene expression and metabolic programs [54].
Sidi Chen developed a system called CLASH that harnesses Cas12a/Cpf1 mRNA and pooled adeno-associated viruses to facilitate simultaneous gene editing and precise transgene knockin using massively parallel homology-directed repair. This system generates a pool of stably integrated mutant variants, each with targeted gene editing. They applied this technology in primary human T cells and observed that mutation of PRDM1 in CAR-T cells resulted in increased proliferation, stem-like properties, central memory, and longevity. Consequently, these cells demonstrated higher efficacy in vivo in CD19 + CD22 + NALM6 cancer models and in the HER2 + HT29 tumor model [55]. (Fig. 3)
The clinical trial for CRISPR-based CAR-T cells
In a Phase I study, CTA101, universal CD19/CD22-targeting CAR-T cells, were infused into patients with r/r ALL. These CAR-T cells featured a CRISPR/Cas9-disrupted TRAC region and CD52 gene to prevent host immune-mediated rejection. On day 28 post-infusion, the complete remission (CR) rate was 83.3%. With a median follow-up of 4.3 months, these CRISPR/Cas9-engineered CAR-T cells displayed a manageable safety profile and significant antileukemia activity. The technology achieved highly efficient, high-fidelity gene editing, resulting in the production of universal CAR-T cells without observable genotoxicity or chromosomal translocations [56].
Utilizing next-generation CRISPR/Cas9 editing, CAR expression was linked to multiplexed DNA editing of TRAC and CD52 by incorporating self-duplicating CRISPR guide RNA expression cassettes within the 3’ long terminal repeat of a CAR19 lentiviral vector. In a study treating children with relapsed/refractory CD19-positive B cell acute lymphoblastic leukemia (B-ALL), six patients received TT52CAR19 T cells. Four of these patients exhibited cell expansion, achieved flow cytometric remission, and subsequently underwent allogeneic stem cell transplantation. While two patients experienced grade II cytokine release syndrome requiring intervention, one patient developed transient grade IV neurotoxicity, and another developed skin GVHD, resolving after transplant conditioning. This study demonstrated the feasibility, safety, and therapeutic potential of CRISPR-engineered immunotherapy [57].
Furthermore, TCR and B2M double-disrupted universal CAR T cells were generated from healthy donor T cells using lentivirus and CRISPR/Cas9 genome-editing technology to treat DLBCL. Although the study had limitations regarding safety and clinical response, the pooled analysis represents a significant advancement in the development of universal CAR T cells for improving safety, efficacy, and feasibility in patients with hematological malignancies [58].
In a single-arm phase I dose-escalation clinical trial evaluating PD1-19bbz in adult patients with r/r B-NHL, twenty-one patients received PD1-19bbz infusion. Most patients had advanced disease stages and intermediate or worse risk stratifications. Notably, some participants exhibited high levels of programmed death ligand-1 (PD-L1) expression in pre-treatment tumor samples. PD1-19bbz demonstrated promising efficacy with a manageable toxicity profile in this first-in-human study of non-viral specifically integrated CAR-T products. A phase I/II trial of PD1-19bbz in a larger patient cohort is currently underway [17].
PD-1-mediated immunosuppression likely limits the efficacy of CAR-T cells in solid tumors. Researchers utilized CRISPR/Cas9 to create PD-1 and TCR deficient mesothelin-specific CAR-T (MPTK-CAR-T) cells and assessed them in a dose-escalation study with 15 patients. No dose-limiting toxicity or unexpected adverse events occurred. Only two patients showed stable disease as the best overall response. Circulating MPTK-CAR-T cells peaked at days 7–14 and declined thereafter. TCR-positive CAR-T cells were predominantly detected post-infusion. Animal models also confirmed the reduced persistence of TCR-deficient CAR-T cells. These findings establish the feasibility and safety of CRISPR-engineered CAR-T cells with PD-1 disruption and underscore the role of natural TCR in CAR-T cell persistence in solid tumor therapy [59].
CAR-T therapy for T cell malignancies faces challenges such as CAR-T cell fratricide and blast contamination. Allogeneic CAR-T cells from healthy donors offer blast-free products but risk graft-versus-host disease (GvHD) and rejection. We developed CD7-targeting CAR-T cells (RD13-01) from healthy donors with genetic modifications for fratricide resistance, GvHD prevention, and enhanced antitumor function. In a phase I trial (NCT04538599) with twelve patients (eleven with T cell leukemia/lymphoma, one with CD7-expressing AML), all met endpoints, with eleven proceeding to efficacy evaluation. No dose-limiting toxicity, GvHD, neurotoxicity, or severe cytokine release syndrome (grade ≥ 3) occurred. At 28 days post-infusion, 81.8% showed objective responses, with a complete response rate of 63.6% (including the AML patient). Three patients underwent allogeneic stem cell transplantation, and four remained in complete remission at a median follow-up of 10.5 months. CMV/EBV reactivation was observed, and one patient died from EBV-associated DLBCL. Expansion of CD7-negative T cells was detected post-infusion. This Phase I trial demonstrates the safety and efficacy of RD13-01 allogeneic CAR-T cells for CD7 + tumors [60].
In Table 3, we summarize the clinical trials of CRISPR- based CAR-T therapies. The clinical trials demonstrate the potential of CRISPR-based CAR-T cell therapy in treating hematological malignancies and solid tumors, but it also presents several challenges in terms of safety and effectiveness.
Conclusion and prospects
The development of the CRISPR system used in human primary T cells has undergone rapid progression over the past decade, especially for gene knockout applications, with relatively high efficiency for both single and multiple gene targeting. Knockout of molecules involved in T cell exhaustion and suppression of T cell function by the CRISPR system can significantly enhance the function of CAR-T cells, providing a new approach for CAR-T cell applications in solid tumors and hematological malignancies.
While CRISPR-based CAR-T cell therapy presents great promise, its application in preclinical studies or clinical trials is fraught with challenges, particularly concerning safety and efficacy. Here, we explore the pivotal safety considerations associated with CRISPR technology and propose potential solutions. (1) Mitigation of Off-Target Effects: The CRISPR system can sometimes induce unwanted mutations at off-target sites within the genome. By employing advanced bioinformatics tools for designing gRNAs and utilizing CRISPR variants with enhanced specificity, the occurrence of off-target effects can be controlled. (2) Immune Response and Immunogenicity: CRISPR-edited cells may trigger immune responses in recipients, potentially leading to rejection or adverse reactions. Strategies to reduce immunogenicity include the selection of non-immunogenic CRISPR components or the use of immunomodulatory agents, which are currently under investigation. (3) Insertional Mutagenesis: Viral vectors used in CRISPR delivery could integrate the CAR gene into the host genome, thereby posing risks of insertional mutagenesis and oncogenesis. Employing non-integrating delivery methods such as mRNA-based or PiggyBac transposon-based approaches can mitigate these risks. (4) Genomic Stability: Ensuring the genomic stability of CRISPR-edited cells is crucial to prevent unintended genetic alterations. Periodic genomic profiling and long-term monitoring of treated patients are essential to assess the stability of edited genomes and to detect any potential abnormalities. (5) Long-Term Effects: Long-term follow-up studies are necessary to evaluate the durability of the therapeutic response and monitor any late-onset adverse events associated with CRISPR-based CAR-T cell therapies. This includes assessing potential long-term effects on the immune system, hematopoiesis, and overall health. Addressing these safety concerns requires rigorous preclinical evaluation, careful patient selection, and continuous monitoring during clinical trials. Another challenge lies in ensuring the efficacy of the treatment, including stable expression of CAR-T cells in the body and their ability to recognize and eliminate tumor cells. This necessitates consideration of the complexities of cellular engineering in the design and optimization of therapeutic protocols and appropriate evaluation and adjustments during clinical trials. Furthermore, the cost and complexity of manufacturing CRISPR-based CAR-T cell therapies pose additional challenges. Optimizing production processes, enhancing the standardization of technology, and reducing manufacturing costs are key factors in advancing this field. In summary, CRISPR-based CAR-T cell therapies hold immense potential in the treatment of various diseases, particularly cancer. While CRISPR/Cas9 remains the most explored system due to its efficiency and relatively better understood characteristics, both CRISPR/Cas12a and CRISPR/Cas13d show promise, each with their unique advantages. The safety and efficacy of these therapies are being actively investigated, and with further research, they can be optimized to provide safer and more effective treatments in the future.
Data availability
No datasets were generated or analysed during the current study.
Change history
23 July 2024
A Correction to this paper has been published: https://doi.org/10.1186/s40364-024-00616-7
Abbreviations
- CAR-T:
-
Chimeric Antigen Receptor T cell
- scFv:
-
Single-Chain Fragment Variable
- B-ALL:
-
B-cell Acute Lymphoblastic Leukemia
- NHL:
-
Non-Hodgkin Lymphoma
- MM:
-
Multiple Myeloma
- LV:
-
Lenti-Virus
- RV:
-
Retroviral Vector
- AAV:
-
Adeno-Associated Virus
- TALENs:
-
Transcription Activator-Like Effector Nucleases
- ZFNs:
-
Zinc-Finger Nucleases
- CRISPR:
-
Clustered Regularly Interspaced Short Palindromic Repeats
- DSB:
-
Double-Stranded Break
- HDR:
-
Homology-Directed Repair
- NHEJ:
-
Non-Homologous End Joining
- sgRNA:
-
Single Guide RNA
- PAM:
-
Protospacer Adjacent Motif
- CRISPRa:
-
CRISPR Activation
- CRISPRi:
-
CRISPR Interference
- PBMCs:
-
Peripheral Blood Mononuclear Cells
- GVHD:
-
Graft-Versus-Host Disease
- HSCT:
-
Hematopoietic Stem Cell Transplant
- TCR:
-
T Cell Receptor
- MHC:
-
Major Histocompatibility Complex
- PSCA:
-
Prostate Stem Cell Antigen
- IRAEs:
-
Immune-Related Adverse Events
- T-ALL:
-
T cell Acute Lymphoblastic Leukemia
- TNF-α:
-
Tumor Necrosis Factor Alpha
- AICD:
-
Activation-Induced Cell Death
- TGFBRI:
-
TGF-β Binds to the TGF-β Receptor
- TGFBR2:
-
TGF Receptor II
- DGK:
-
Glycerol Diglyceride Kinase
- GM-CSF:
-
Granulocyte Macrophage Colony Stimulating Factor
- CRS:
-
Cytokine Release Syndrome
- dsDNA:
-
Double-Stranded DNA
- SB:
-
Sleeping Beauty
- GBM:
-
Glioblastoma
- TPEX:
-
Precursor Exhausted T Cells
- RasGAP:
-
RAS GTPase-Activating Protein
- dgRNA:
-
Dead-Guide RNA
- OMEGA:
-
Obligate Mobile Element-Guided Activity Omega
- GMP:
-
Good Manufacturing Practice
References
Eshhar Z, Waks T, Gross G, Schindler DG. Specific activation and targeting of cytotoxic lymphocytes through chimeric single chains consisting of antibody-binding domains and the gamma or zeta subunits of the immunoglobulin and T-cell receptors. Proc Natl Acad Sci U S A. 1993;90:720–4.
Bailey SR, Maus MV. Gene editing for immune cell therapies. Nat Biotechnol. 2019;37:1425–34.
Urnov FD, Rebar EJ, Holmes MC, Zhang HS, Gregory PD. Genome editing with engineered zinc finger nucleases. Nat Rev Genet. 2010;11:636–46.
Katsuyama T, Akmammedov A, Seimiya M, Hess SC, Sievers C, Paro R. An efficient strategy for TALEN-mediated genome engineering in Drosophila. Nucleic Acids Res. 2013;41:e163.
Palpant NJ, Dudzinski D. Zinc finger nucleases: looking toward translation. Gene Ther. 2013;20:121–7.
Gaj T, Gersbach CA, Barbas CF 3. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 2013;31:397–405.
Hsu PD, Lander ES, Zhang F. Development and applications of CRISPR-Cas9 for genome engineering. Cell. 2014;157:1262–78.
Tieu V, Sotillo E, Bjelajac JR, Chen C, Malipatlolla M, Guerrero JA, Xu P, Quinn PJ, Fisher C, Klysz D, et al. A versatile CRISPR-Cas13d platform for multiplexed transcriptomic regulation and metabolic engineering in primary human T cells. Cell. 2024;187:1278–e12951220.
Dong MB, Tang K, Zhou X, Zhou JJ, Chen S. Tumor immunology CRISPR screening: present, past, and future. Trends Cancer. 2022;8:210–25.
Roth TL, Puig-Saus C, Yu R, Shifrut E, Carnevale J, Li PJ, Hiatt J, Saco J, Krystofinski P, Li H, et al. Reprogramming human T cell function and specificity with non-viral genome targeting. Nature. 2018;559:405–9.
Choi BD, Yu X, Castano AP, Darr H, Henderson DB, Bouffard AA, Larson RC, Scarfo I, Bailey SR, Gerhard GM, et al. CRISPR-Cas9 disruption of PD-1 enhances activity of universal EGFRvIII CAR T cells in a preclinical model of human glioblastoma. J Immunother Cancer. 2019;7:304.
Hendel A, Bak RO, Clark JT, Kennedy AB, Ryan DE, Roy S, Steinfeld I, Lunstad BD, Kaiser RJ, Wilkens AB, et al. Chemically modified guide RNAs enhance CRISPR-Cas genome editing in human primary cells. Nat Biotechnol. 2015;33:985–9.
Kim HK, Song M, Lee J, Menon AV, Jung S, Kang YM, Choi JW, Woo E, Koh HC, Nam JW, Kim H. In vivo high-throughput profiling of CRISPR-Cpf1 activity. Nat Methods. 2017;14:153–9.
Dai X, Park JJ, Du Y, Kim HR, Wang G, Errami Y, Chen S. One-step generation of modular CAR-T cells with AAV-Cpf1. Nat Methods. 2019;16:247–54.
Zhang L, Zuris JA, Viswanathan R, Edelstein JN, Turk R, Thommandru B, Rube HT, Glenn SE, Collingwood MA, Bode NM, et al. AsCas12a ultra nuclease facilitates the rapid generation of therapeutic cell medicines. Nat Commun. 2021;12:3908.
Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJ, Hamieh M, Cunanan KM, Odak A, Gonen M, Sadelain M. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature. 2017;543:113–7.
Zhang J, Hu Y, Yang J, Li W, Zhang M, Wang Q, Zhang L, Wei G, Tian Y, Zhao K, et al. Non-viral, specifically targeted CAR-T cells achieve high safety and efficacy in B-NHL. Nature. 2022;609:369–74.
Jing R, Jiao P, Chen J, Meng X, Wu X, Duan Y, Shang K, Qian L, Huang Y, Liu J, et al. Cas9-Cleavage sequences in size-reduced plasmids enhance nonviral genome targeting of CARs in primary human T cells. Small Methods. 2021;5:e2100071.
Nguyen DN, Roth TL, Li PJ, Chen PA, Apathy R, Mamedov MR, Vo LT, Tobin VR, Goodman D, Shifrut E, et al. Polymer-stabilized Cas9 nanoparticles and modified repair templates increase genome editing efficiency. Nat Biotechnol. 2020;38:44–9.
Depil S, Duchateau P, Grupp SA, Mufti G, Poirot L. Off-the-shelf’ allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov. 2020;19:185–99.
Stenger D, Stief TA, Kaeuferle T, Willier S, Rataj F, Schober K, Vick B, Lotfi R, Wagner B, Grunewald TGP, et al. Endogenous TCR promotes in vivo persistence of CD19-CAR-T cells compared to a CRISPR/Cas9-mediated TCR knockout CAR. Blood. 2020;136:1407–18.
Cherkassky L, Morello A, Villena-Vargas J, Feng Y, Dimitrov DS, Jones DR, Sadelain M, Adusumilli PS. Human CAR T cells with cell-intrinsic PD-1 checkpoint blockade resist tumor-mediated inhibition. J Clin Invest. 2016;126:3130–44.
Amezquita RA, Kaech SM. Immunology: the chronicles of T-cell exhaustion. Nature. 2017;543:190–1.
Wherry EJ, Kurachi M. Molecular and cellular insights into T cell exhaustion. Nat Rev Immunol. 2015;15:486–99.
Baumeister SH, Freeman GJ, Dranoff G, Sharpe AH. Coinhibitory pathways in Immunotherapy for Cancer. Annu Rev Immunol. 2016;34:539–73.
Cao Y, Lu W, Sun R, Jin X, Cheng L, He X, Wang L, Yuan T, Lyu C, Zhao M. Anti-CD19 Chimeric Antigen Receptor T Cells in Combination with Nivolumab are safe and effective against Relapsed/Refractory B-Cell non-hodgkin Lymphoma. Front Oncol. 2019;9:767.
Chong EA, Melenhorst JJ, Lacey SF, Ambrose DE, Gonzalez V, Levine BL, June CH, Schuster SJ. PD-1 blockade modulates chimeric antigen receptor (CAR)-modified T cells: refueling the CAR. Blood. 2017;129:1039–41.
Ramos-Casals M, Brahmer JR, Callahan MK, Flores-Chavez A, Keegan N, Khamashta MA, Lambotte O, Mariette X, Prat A, Suarez-Almazor ME. Immune-related adverse events of checkpoint inhibitors. Nat Rev Dis Primers. 2020;6:38.
Hu W, Zi Z, Jin Y, Li G, Shao K, Cai Q, Ma X, Wei F. CRISPR/Cas9-mediated PD-1 disruption enhances human mesothelin-targeted CAR T cell effector functions. Cancer Immunol Immunother. 2019;68:365–77.
Ren J, Zhang X, Liu X, Fang C, Jiang S, June CH, Zhao Y. A versatile system for rapid multiplex genome-edited CAR T cell generation. Oncotarget. 2017;8:17002–11.
Zhang Y, Zhang X, Cheng C, Mu W, Liu X, Li N, Wei X, Liu X, Xia C, Wang H. CRISPR-Cas9 mediated LAG-3 disruption in CAR-T cells. Front Med. 2017;11:554–62.
Campana D, van Dongen JJ, Mehta A, Coustan-Smith E, Wolvers-Tettero IL, Ganeshaguru K, Janossy G. Stages of T-cell receptor protein expression in T-cell acute lymphoblastic leukemia. Blood. 1991;77:1546–54.
Chen KH, Wada M, Pinz KG, Liu H, Lin KW, Jares A, Firor AE, Shuai X, Salman H, Golightly M, et al. Preclinical targeting of aggressive T-cell malignancies using anti-CD5 chimeric antigen receptor. Leukemia. 2017;31:2151–60.
Dai Z, Mu W, Zhao Y, Cheng J, Lin H, Ouyang K, Jia X, Liu J, Wei Q, Wang M, et al. T cells expressing CD5/CD7 bispecific chimeric antigen receptors with fully human heavy-chain-only domains mitigate tumor antigen escape. Signal Transduct Target Ther. 2022;7:85.
Dai Z, Mu W, Zhao Y, Jia X, Liu J, Wei Q, Tan T, Zhou J. The rational development of CD5-targeting biepitopic CARs with fully human heavy-chain-only antigen recognition domains. Mol Ther. 2021;29:2707–22.
Benyahia B, Bensaid Y, Ammar F, Dhobb M, Benjelloun A, Benabderrazik T. [Arteriopathies of the lower limbs in adults under 40 years of age]. Chirurgie. 1989;115(Suppl 1):18–26. discussion 26 – 17.
Lu Y, Xue J, Deng T, Zhou X, Yu K, Deng L, Huang M, Yi X, Liang M, Wang Y, et al. Safety and feasibility of CRISPR-edited T cells in patients with refractory non-small-cell lung cancer. Nat Med. 2020;26:732–40.
Pickup M, Novitskiy S, Moses HL. The roles of TGFbeta in the tumour microenvironment. Nat Rev Cancer. 2013;13:788–99.
Tang N, Cheng C, Zhang X, Qiao M, Li N, Mu W, Wei XF, Han W, Wang H. TGF-beta inhibition via CRISPR promotes the long-term efficacy of CAR T cells against solid tumors. JCI Insight 2020, 5.
Giuffrida L, Sek K, Henderson MA, Lai J, Chen AXY, Meyran D, Todd KL, Petley EV, Mardiana S, Molck C, et al. CRISPR/Cas9 mediated deletion of the adenosine A2A receptor enhances CAR T cell efficacy. Nat Commun. 2021;12:3236.
Jung IY, Kim YY, Yu HS, Lee M, Kim S, Lee J. CRISPR/Cas9-Mediated knockout of DGK improves Antitumor activities of Human T cells. Cancer Res. 2018;78:4692–703.
Sterner RM, Sakemura R, Cox MJ, Yang N, Khadka RH, Forsman CL, Hansen MJ, Jin F, Ayasoufi K, Hefazi M, et al. GM-CSF inhibition reduces cytokine release syndrome and neuroinflammation but enhances CAR-T cell function in xenografts. Blood. 2019;133:697–709.
Yi Y, Chai X, Zheng L, Zhang Y, Shen J, Hu B, Tao G. CRISPR-edited CART with GM-CSF knockout and auto secretion of IL6 and IL1 blockers in patients with hematologic malignancy. Cell Discov. 2021;7:27.
Wang D, Zhang F, Gao G. CRISPR-Based therapeutic genome editing: strategies and in vivo delivery by AAV vectors. Cell. 2020;181:136–50.
Patel SJ, Sanjana NE, Kishton RJ, Eidizadeh A, Vodnala SK, Cam M, Gartner JJ, Jia L, Steinberg SM, Yamamoto TN, et al. Identification of essential genes for cancer immunotherapy. Nature. 2017;548:537–42.
Joung J, Konermann S, Gootenberg JS, Abudayyeh OO, Platt RJ, Brigham MD, Sanjana NE, Zhang F. Genome-scale CRISPR-Cas9 knockout and transcriptional activation screening. Nat Protoc. 2017;12:828–63.
Ye L, Park JJ, Dong MB, Yang Q, Chow RD, Peng L, Du Y, Guo J, Dai X, Wang G, et al. In vivo CRISPR screening in CD8 T cells with AAV-Sleeping Beauty hybrid vectors identifies membrane targets for improving immunotherapy for glioblastoma. Nat Biotechnol. 2019;37:1302–13.
Wei J, Long L, Zheng W, Dhungana Y, Lim SA, Guy C, Wang Y, Wang YD, Qian C, Xu B, et al. Targeting REGNASE-1 programs long-lived effector T cells for cancer therapy. Nature. 2019;576:471–6.
Zheng W, Wei J, Zebley CC, Jones LL, Dhungana Y, Wang YD, Mavuluri J, Long L, Fan Y, Youngblood B, et al. Regnase-1 suppresses TCF-1 + precursor exhausted T-cell formation to limit CAR-T-cell responses against ALL. Blood. 2021;138:122–35.
Carnevale J, Shifrut E, Kale N, Nyberg WA, Blaeschke F, Chen YY, Li Z, Bapat SP, Diolaiti ME, O’Leary P, et al. RASA2 ablation in T cells boosts antigen sensitivity and long-term function. Nature. 2022;609:174–82.
Freitas KA, Belk JA, Sotillo E, Quinn PJ, Ramello MC, Malipatlolla M, Daniel B, Sandor K, Klysz D, Bjelajac J, et al. Enhanced T cell effector activity by targeting the mediator kinase module. Science. 2022;378:eabn5647.
Wang D, Prager BC, Gimple RC, Aguilar B, Alizadeh D, Tang H, Lv D, Starr R, Brito A, Wu Q, et al. CRISPR Screening of CAR T cells and Cancer stem cells reveals critical dependencies for cell-based therapies. Cancer Discov. 2021;11:1192–211.
Guo A, Huang H, Zhu Z, Chen MJ, Shi H, Yuan S, Sharma P, Connelly JP, Liedmann S, Dhungana Y, et al. cBAF complex components and MYC cooperate early in CD8(+) T cell fate. Nature. 2022;607:135–41.
Ye L, Park JJ, Peng L, Yang Q, Chow RD, Dong MB, Lam SZ, Guo J, Tang E, Zhang Y, et al. A genome-scale gain-of-function CRISPR screen in CD8 T cells identifies proline metabolism as a means to enhance CAR-T therapy. Cell Metab. 2022;34:595–e614514.
Dai X, Park JJ, Du Y, Na Z, Lam SZ, Chow RD, Renauer PA, Gu J, Xin S, Chu Z et al. Massively parallel knock-in engineering of human T cells. Nat Biotechnol 2023.
Hu Y, Zhou Y, Zhang M, Ge W, Li Y, Yang L, Wei G, Han L, Wang H, Yu S, et al. CRISPR/Cas9-Engineered Universal CD19/CD22 Dual-targeted CAR-T cell therapy for Relapsed/Refractory B-cell Acute Lymphoblastic Leukemia. Clin Cancer Res. 2021;27:2764–72.
Ottaviano G, Georgiadis C, Gkazi SA, Syed F, Zhan H, Etuk A, Preece R, Chu J, Kubat A, Adams S, et al. Phase 1 clinical trial of CRISPR-engineered CAR19 universal T cells for treatment of children with refractory B cell leukemia. Sci Transl Med. 2022;14:eabq3010.
Guo Y, Tong C, Su L, Zhang W, Jia H, Liu Y, Yang Q, Wu Z, Wang Y, Han W. CRISPR/Cas9 genome-edited universal CAR T cells in patients with relapsed/refractory lymphoma. Blood Adv. 2022;6:2695–9.
Wang Z, Li N, Feng K, Chen M, Zhang Y, Liu Y, Yang Q, Nie J, Tang N, Zhang X, et al. Phase I study of CAR-T cells with PD-1 and TCR disruption in mesothelin-positive solid tumors. Cell Mol Immunol. 2021;18:2188–98.
Hu Y, Zhou Y, Zhang M, Zhao H, Wei G, Ge W, Cui Q, Mu Q, Chen G, Han L, et al. Genetically modified CD7-targeting allogeneic CAR-T cell therapy with enhanced efficacy for relapsed/refractory CD7-positive hematological malignancies: a phase I clinical study. Cell Res. 2022;32:995–1007.
Acknowledgements
Not applicable.
Funding
This study was funded by the medical and health research project of Zhejiang province (grant numbers: 2024KY1312), Zhejiang Provincial Basic Public Welfare Research Project (grant number: LGF22H160082), Zhejiang Medical and Health Science and Technology Plan Project (grant number:2022KY939) and Hangzhou Medical and Health Science and Technology Major Project (grant number: Z20210025).
Author information
Authors and Affiliations
Contributions
D.L. and R.J. initiated the project and devised the main conceptual ideas. P.S., R.J., Q.Z., Z.X., and Y.S. drafted and revised the manuscript. All authors reviewed and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, P., Zhang, Q., Xu, Z. et al. CRISPR/Cas-based CAR-T cells: production and application. Biomark Res 12, 54 (2024). https://doi.org/10.1186/s40364-024-00602-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-024-00602-z